Abstract

Background: Thrombopoietin receptor agonists(TPO-RAs) have been thought to play only a supporting role in ITP management. Several retrospective studies and a recent prospective study have reported unexpected cases of durable remission after TPO-RAs discontinuation in adult ITP in up to 30%. However, newly diagnosed ITP cases for which spontaneous remission may occur have been included in most of these studies. Thus, the main purpose of this study was to determine the proportion of patients with either persistent or chronic phase and no recent exposure to any potentially curative therapy (i.e., splenectomy or rituximab) achieving long-term remission off-treatment at 24 and 52 months after at least 3 months of TPO-RAs exposure with a complete response (CR).
Patients/methods: We conducted a nationwide prospective multicenter interventional study (NCT03119974). Inclusion criteria were: 1) Patients aged > 18 years, with persistent or chronic primary ITP, 2) A stable CR defined by a platelet count > 100 x 10 9/L for more than 2 months on TPO-RA therapy, 3) Treatment with TPO-RA for at least 3 months. Main exclusion criteria were: 1) Anticoagulation or anti-platelet treatment, 2) Previous failure of TPO-RA discontinuation, 3) Concomitant treatment with corticosteroids ± intravenous immunoglobulin 4) Rituximab or splenectomy within the 2 months preceding or after TPO-RA initiation. After inclusion, the decrease and wean of either eltrombopag or romiplostim was initiated according to a standardized protocol (respectively tapering of 25 mg every 2 weeks or tapering of 1 ug/kg every week). In any case TPO-RAs had to be stopped at week 10. In case of relapse after TPO-RA discontinuation, the decision to start a new therapy was left at every investigator discretion. The primary endpoint was the proportion of patients achieving an overall response (CR + R) at week 24 (6 months) after TPO-RAs discontinuation. Secondary outcomes were overall response rate over the study period (W52), bleeding events, and to identify predictive factors, for overall prolonged response (W24 and W52).
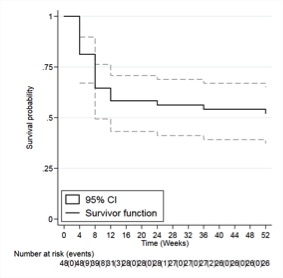
Results: Forty-nine patients (30 females, 61%), with persistent (n=2) or chronic (n=47, 96%) chronic ITP, with a median age of 58.5 years IQR (41 to 73) fulfilling the eligibility criteria were included over 2 year-period in 22 centers from the French reference network for adult' ITP. Forty patients received eltrombopag and 9 romiplostim at the time of inclusion. One patient was excluded since she was diagnosed pregnant one day after inclusion. In intention to treat 27/48 (56.2%; 95% CI, 29.5 to 58.8) patients achieved the primary-endpoint and maintained an overall response at week 24 after TPO-RAS discontinuation with a complete response for 15/27 (55%). During the full follow-up period of 52 weeks after TPO-RAs discontinuation, overall response was observed in 25/48 (52.1%; 95% CI, 37.2 to 66.2) patients (Figure 1). Bleeding events occurred in 13/21 (61.9%) and 15/23 (65.2%) patients relapsing respectively at 24 and 52 months with a median platelet count of 31´10 9/L(26 to 39) and 31 ´10 9/L(23 to 39). No severe bleeding episode (French bleeding score > 8) occurred. Median time of relapse after tapering initiation was 8 weeks. Among 21 patients with a relapse (<30 x 10 9/L) before week 24, 13 patients were re-challenged with the same TPO-RA with a CR achieved with a median time of 2 weeks (2-4). In univariate analysis, age, ITP duration, TPO-RA duration before discontinuation, platelet count at inclusion and TPO-RAs drug class were not predictive of sustained response.
Conclusion: These results showed an unexpectedly high rate of sustained off-treatment remission after TPO-RAs discontinuation in chronic ITP among patients who initially achieve a stable CR. When they occur, relapses are mainly observed within the first weeks after discontinuation, very rarely afterwards and with no severe bleeding. While no predictive factor of lasting remission has been yet identified, our study strongly supports a progressive tapering of the dose of TPO-RAs in patients achieving a stable CR on treatment.
Figure 1: Relapse at 52 weeks after TPO-RAs discontinuation
Mahevas: GSK: Research Funding; Amgen: Honoraria. Viallard: Novartis: Consultancy; Grifols: Consultancy; LFB: Consultancy; Amgen: Consultancy. Moulis: Amgen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Argenx: Membership on an entity's Board of Directors or advisory committees; Grifols: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Sobi: Membership on an entity's Board of Directors or advisory committees. Terriou: Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Michel: Novartis: Consultancy; Amgen: Consultancy; UCB: Honoraria; Argenx: Honoraria; Rigel: Honoraria; Alexion: Honoraria. Godeau: Sobi: Consultancy; Novartis: Consultancy; Amgen: Consultancy; Grifols: Consultancy.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal